Preserving the Optic Nerve with coMra therapy
A non-invasive, in-office approach to vision protection and functional recovery
Why it matters
The optic nerve rarely regenerates — and by the time visual field loss is noticed, a substantial portion of axons may already be gone. In glaucoma, ischemic neuropathy, post-stroke suppression, or optic neuritis, conventional care can stabilize but rarely restore function. coMra therapy offers an adjunctive path: safe, painless, and designed to preserve function and activate repair without thermal, phototoxic, or excitatory overstimulation.
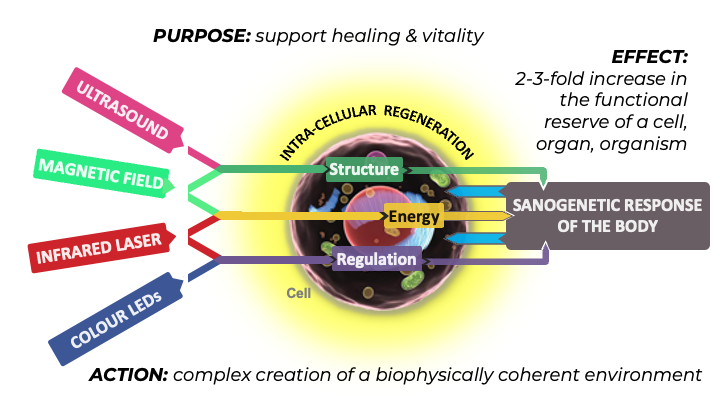
The coMra therapy approach
coMra ❓ therapy delivers low-level infrared laser, low-frequency ultrasound, a magnetic field, and sequenced color light together as one coherent signal — designed to:
- Support mitochondrial energy and axonal transport
- Promote neuroprotection and microcirculation
- Reduce inflammation and oxidative stress
- Facilitate functional recovery in damaged pathways
🧠 Biological Rationale
The optic nerve and its pathways are among the most metabolically active tissues in the body — dependent on uninterrupted mitochondrial ATP production, efficient microvascular perfusion, and balanced neuroimmune regulation.
coMra therapy’s low-intensity, coherent stimulation:
- Enhances mitochondrial ATP production → sustaining axonal transport and synaptic activity
- Promotes neurotrophic factor expression → aiding repair and neuroplasticity in damaged pathways
- Improves microcirculation → ensuring steady oxygen and nutrient delivery
- Modulates inflammatory and oxidative stress pathways → protecting against secondary degeneration
These effects occur without thermal or phototoxic injury, enabling safe, repeatable application in ocular and periocular regions.
📚 Supporting Research
“Selected studies documenting biological mechanisms relevant to optic nerve support and ocular tissue repair.”
- Mitochondrial energy & neuroprotection — Kamenskikh et al.: Restoration of mitochondrial homeostasis and blood–ocular barrier function in degenerative eye disease
- Neurotrophic factor expression — Egorov et al.: Photobiomodulation-induced neurotrophic support in retinal and optic nerve pathology
- Microcirculation enhancement — Novikova (2011): Visual field preservation in POAG via ultrasound stimulation of ocular blood flow
- Tissue regeneration — Radnaeva (2007): Magneto-infrared-laser–assisted corneal regeneration in complex injury cases
🔬 Clinical outcomes (snapshot)
| Case | Condition | Result |
|---|---|---|
| 68F | Post-stroke visual field loss + suppression | Full binocular fusion; expanded field |
| 54F | Optic neuritis (non-MS) | Improved VA, contrast sensitivity; field stability |
| 71M | Diabetic ischemia (OS) | Visual field expanded >2.5× in weeks |
| 49F | Sixth nerve paralysis (post brain-tumor surgery) | Full eye movement and alignment restored |
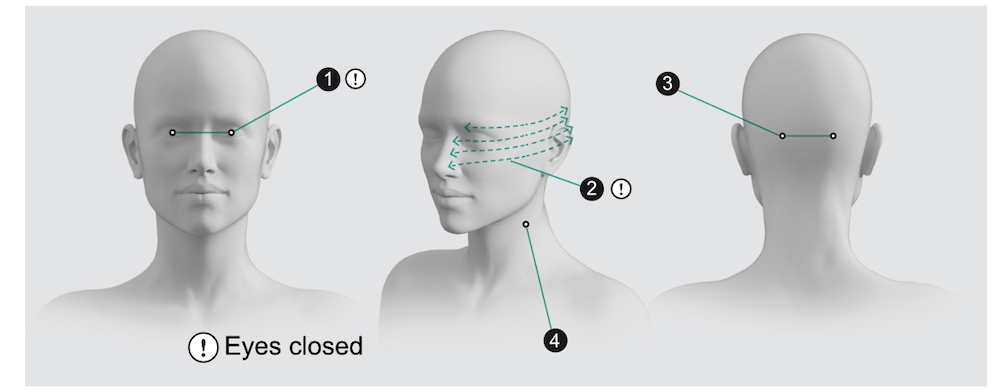
Optic Nerve Health — Eye Protocol (base)
For complete instructions, see Eye Protocol
| Step | Area treated | Time | Frequency / Program |
|---|---|---|---|
| 1 | Closed eye (directly over lid) | 2 min per eye | per protocol |
| 2 | Facial scan (eye + optic nerve pathway) | 5 min per side | per protocol |
| 3 | Occipital area (visual cortex) | 1 min per side | per protocol |
| 4 | Carotid band (side of neck) | 2 min per side | per protocol |
Typical Total Time: ~20 min before adjustments
Session frequency: adapt to your clinical model (weekly, biweekly, or integrated with existing therapy blocks)
⚠️ Safety & Integration
- When treating on or near the eyes (Steps 1 & 2), always ensure eyes are gently closed.
- coMra is non-thermal and will not cause tissue damage.
- Safe, adjunctive, and compatible with technician-led delivery.
- Pairs well with vision therapy, syntonics, microcurrent, rehab, and metabolic care.
Whether you’re exploring options, already own a device, or want to train staff — we’ll help you integrate effectively.